Reforming Cancer MDT Meetings Across Greater Manchester
Multidisciplinary Team Meetings (MDTMs) are a well-established aspect of cancer care and have been regarded as gold standard practice since the Calman-Hine report of 1995 and the NHS National Cancer Plan in 2000. Over the past 25 years, there has been little change to the format of MDTMs despite significant changes in cancer care. A need for significant change was supported by Cancer Research UK in 2017 and confirmed by NHS Improvement in 2020.
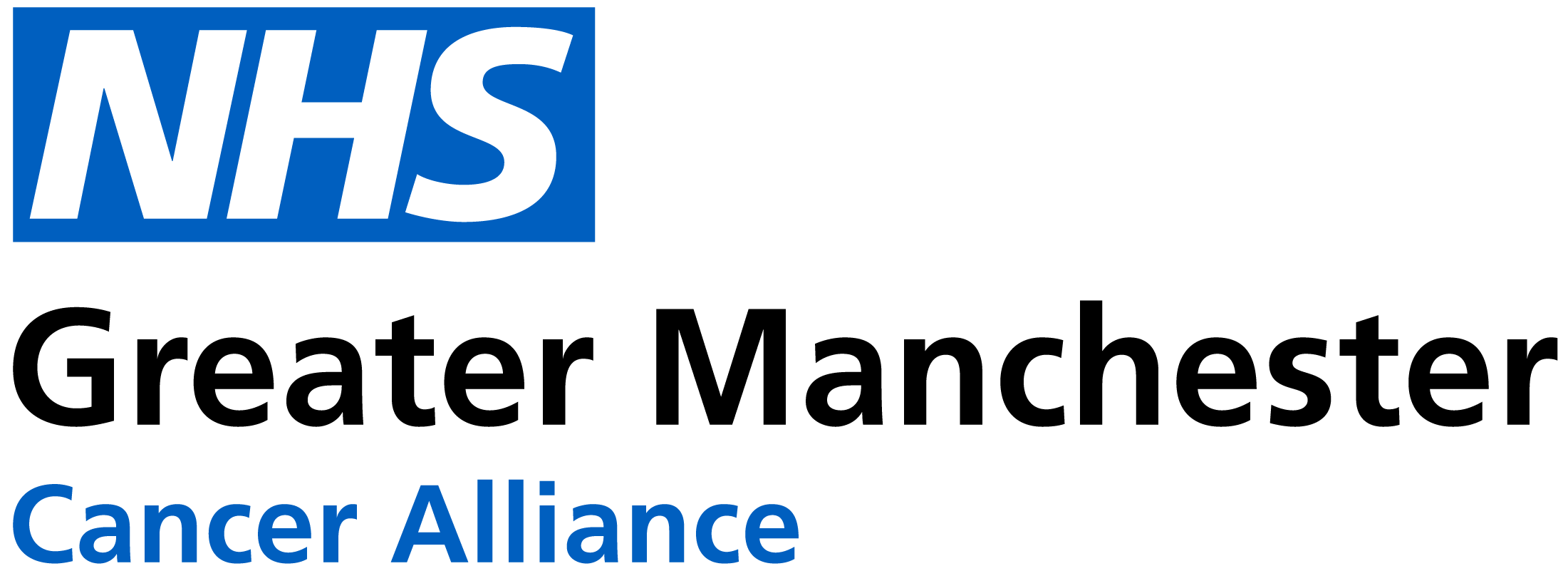
It is agreed that by improving communication and documentation between team members and adopting a more streamlined approach to MDTMs, there is significant potential to release clinician time, which could then be repurposed elsewhere in patient care.
To support this, an MDT Reform Programme of work has been developed following an 18 month MDT Reform Project with a dedicated project group and Clinical Lead. This has led to the development of agreed, co-produced Greater Manchester MDTM Standards detailing what principles should be central to Cancer MDT working across the Region, with examples of good practice, to encourage shared, peer-peer learning, and continued reform.
The 10 principles within the standards
Keeping the patient at the heart of MDT reform
During the project we worked collaboratively with patient representatives to co-produce patient resources.