The NHS Long Term Plan ambitions for early cancer diagnosis are: by 2028, 75% of people with cancer will be diagnosed at an early stage (stage 1 or 2) and 55,000 more people each year will survive their cancer for five years.
Earlier and faster diagnosis of cancer is dependent on people understanding and being aware of the early signs and symptoms of cancer, by taking up screening programmes or visiting a healthcare professional. Healthcare professionals must also be aware of and have the tools to hand to ensure a timely referral.
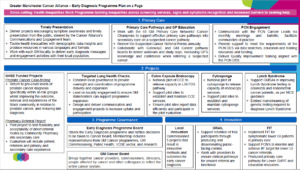
A programme of work has been established on behalf of GM Cancer Alliance and the GM system to support the delivery of the NHS Long Term Plan early cancer diagnosis ambition.
Early Diagnosis Programme of Work
Communications and Engagement
The Cancer Alliance Communications and Engagement team play a key role in delivering early diagnosis projects encouraging symptom awareness and timely presentation from the public in the following ways:
- Tackle health inequalities using demographic data insights to target advertising and reduce barriers to presentation.
- Produce resources in various languages and formats suitable for audiences with additional needs.
- Work with local teams in each GM locality to deliver early diagnosis messages and engagement activities suited to the needs of their community.
- Monitor the reach and engagement of people from the most deprived communities in Greater Manchester, and communities identified to be a priority through data and insight work.
Greater Manchester Locality Engagement
We are commissioning the 10 GM localities to deliver early diagnosis communication and engagement work with specific communities in their areas.
VCSE Engagement
Our VCSE Strategic Lead for Cancer and Inequalities channels the voices and insights from a broad range of marginalised communities into decisions taken at a regional level through the Early Diagnosis Programme Board.
Primary Care Network (PCN) Engagement
We have developed a network of support with the 65 Primary Care Networks in Greater Manchester by establishing a “Cancer Lead” role in each PCN – a primary care professional in general practice responsible for leading on early diagnosis initiatives in their PCN’s area.
PCN Direct Enhanced Service (DES)
We consistently engage with the network of PCN Cancer Leads through our monthly PCN Bulletin and meetings.
We also developed our support offers as an Alliance to assist with delivery of the annual PCN DES for early cancer diagnosis, especially within the most deprived areas where late stage diagnosis is more prevalent.
Read the NHSE PCN DES Early Cancer Diagnosis Support Pack 2023/24.
Suspected Cancer Referral Forms
Every year, with the steer of GM Cancer Pathway Boards and adherence to NG12 NICE guidance, we update the Suspected Cancer Referral Forms for General Practice. These are uploaded onto every GP system in GM by the GM Data Quality Team for GPs to refer a patient onto a cancer pathway into secondary care.
To increase GP confidence when identifying cancer symptoms and referring a patient for a suspected cancer, we collaborate with GatewayC and GM Cancer pathway board clinicians to deliver webinars and study days on tumour specific and non-symptom specific topics.
FIT
The use of FIT for symptomatic patients on the Lower GI is a priority for Cancer Alliances to deliver and will lead to earlier and faster diagnosis of Lower GI cancers as well as a reduction in the amount of colonoscopies undertaken.
To date, our work with Primary Care to increase the percentage of FIT results sent with a Lower GI referral form, as per BSG and NICE guidance recommendations includes:
- Developing and monitoring IIF indicators for FIT data, collaborating with PCN Cancer Leads and the GM Cancer BI team.
- Producing a range of GP and patient facing educational materials including webinars, infographics and podcasts.
- Developing a Primary Care Pathway for positive and negative FIT results, ensuring patient follow up and safety netting is prioritised.
Local Innovation
The Cancer Alliance commissioned five projects following a multi-stage judging panel process reviewing project proposal bids. Details will be made available as the projects progress.
Health inequalities are avoidable, unfair and systematic differences in health between different groups of people. They exist as a result of systematic variation in (i) the accessibility, quality and experience of health and care services, (ii) individual behaviours and, most importantly, (iii) the wider determinants of health, such as employment, education and income.
Health inequalities in the cancer system can represent themselves as differences between groups in:
- the risk of getting cancer
- the proportion of people diagnosed at an early stage
- access and experience of diagnosis, treatment, and care
- access to and representation within research
- representation within the workforce
At GM Cancer we are committed to tackling inequalities in cancer incidence and outcomes and improve equity in access and experience of cancer care. Click here to find out more about our work tackling health inequalities.
Projects
The aim of the Targeted Lung Health Check programme is to detect lung cancer and disease early so that people can be treated sooner and more effectively – saving more lives.
Lung cancer often has no symptoms in the earlier stages which can result in it not being found until the later stages when outcomes are less favourable.
In June 2023, the Government announced that TLHCs was now a national screening programme, which would roll out to cover the whole of the country over the next several years. You can read this announcement here.
For more information, please read our FAQ’s below or visit our provider’s website www.mft.nhs.uk/lunghealthcheck/.
Q. What is a Targeted Lung Health Check?
A. The lung health check takes part in two stages. The first is an appointment with a specially trained nurse to assess your risk level. If you are found to be at high risk of having lung cancer you will be eligible for a low dose CT scan so we can capture an image of your lungs and identify if there are any issues which need further investigation or treatment.
Q. Where will lung health checks take place?
A. The lung health check appointment and CT scan will take place in a mobile unit. The mobile units will be parked in community venues or supermarket car parks which have good transport links for ease of access.
Q. Who is eligible?
A. People aged 55 to 74 years old who are current or former smokers are eligible to take participate in the programme.
Q. How will people be invited to the programme?
A. People will be invited to the programme based on the GP practice where they are registered. Everybody in the age range will be invited but only current or former smokers will be eligible for an appointment.
Q. When will the TLHC programme be in my area?
A. The Greater Manchester TLHC programme is currently available in Salford, North Manchester, and Tameside. The Greater Manchester Cancer Alliance is working hard to expand the programme to all eligible residents by 2028.
Q. I’m not eligible for the programme but concerned about my health, what should I do?
A. This is a targeted screening programme and people between 55 – 74 and have smoked more than 100 cigarettes in their lifetime are eligible. If you are worried about any of the below symptoms, please see your GP as soon as possible:
-
- A persistent cough or change in your normal cough
- Coughing up blood
- Being short of breath
- Unexplained tiredness or weight loss
- An ache or pain when breathing or coughing
- Appetite loss
Q. I’m a healthcare professional who would like more information about the programme, who should I contact?
A. Thank you for your interest in the programme. If you would like any additional resources or information to support the rollout of targeted lung health checks in your area, please contact oliver.butterworth2@nhs.net (TLHC Project Manager).
The aim of the Prostate Pilot is to detect prostate cancer and disease early so that people can be treated sooner and more effectively – saving more lives.
Prostate cancer is the most common cancer in men, but most men with early prostate cancer don’t have any symptoms. This Van Can is our Greater Manchester NHS mobile health clinic which is raising awareness of Prostate Cancer.
The van is also open to all other men and people with a prostate aged over 45 who have a family history of prostate, breast or ovarian cancer. This means your father or brother has had prostate cancer when they were under the age of 55 or your mother or sister has had breast or ovarian cancer when they were under the age of 50. This is because family history can also increase your risk of developing prostate cancer.
For more information, please read visit our website www.thisvancan.co.uk
Q. How do I visit the van?
A. You will need to make an appointment to visit the van either by phone or email. The contact details are listed on our website www.thisvancan.co.uk
Q. What happens on the van?
A. When you turn up, you will be able to talk to a member of NHS staff, privately and in a relaxed environment. Our NHS staff will talk to you about your risk of prostate cancer, answer any questions that you might have and provide information about your prostate health.
You can then also choose whether to have a free Prostate Specific Antigen (PSA) blood test. If you decide to go ahead and have a PSA blood test, we will take a blood sample from your arm, whilst you are in in the van. We will get back to you with your results within a few weeks. If you need any further tests, we’ll let you know.
Q. Who is eligible?
A. The service is for men, or people with a prostate, who fit the following criteria:
- black and over age 45
- if you have a family history of prostate, breast or ovarian cancer and are over 45. This means your father or brother has had prostate cancer when they were under the age of 55 or your mother or sister has had breast or ovarian cancer when they were under the age of 50.
Q. How will people be invited to the programme?
A. People will be invited to the programme based on the GP practice where they are registered. Everybody who fits the above criteria will be invited to visit the van.
Q. I’m not eligible for the programme but concerned about my health, what should I do?
A. If you are over 50 and worried about your risk of prostate cancer but do not fit the criteria to visit ThisVanCan we encourage you to contact your GP to discuss further.
You can also check your risk of prostate cancer by using the Prostate Cancer UK risk checker at Check your risk in 30 seconds | Prostate Cancer UK
Q. I’m a healthcare professional who would like more information about the programme, who should I contact?
A. Thank you for your interest in the programme. If you would like any additional resources or information to support the rollout of This Van Can in your area, please contact millie.wadley1@nhs.net (Project Manager).
Colon Capsule Endoscopy (CCE) is a procedure that uses a camera to examine the large bowel. The aim of the pilot is to evaluate the diagnostic accuracy of CCE in patients at risk of colorectal cancer or undergoing post-polypectomy bowel surveillance.
The test involves swallowing a small pill that contains a small disposable camera, which travels along your gut and takes thousands of pictures. These are transmitted to a data recorder that you wear on your waist. This is an alternative to an invasive colonoscopy.
Q. Where is CCE available?
A. CCE is currently only available in Salford Royal Hospital and Royal Oldham Hospital. As we are still in the pilot stage, it is not available across the whole of Greater Manchester.
Q. Who is eligible?
A. People who have been referred by their GP on an urgent cancer pathway to the symptomatic endoscopy service, with a FIT score of 10-100ug/gm.
Q. I’m a healthcare professional who would like more information about the programme, who should I contact?
A. Thank you for your interest in the pilot. If you would like any additional resources or information, please contact s.walker21@nhs.net
Capsule Sponge is a procedure where a small capsule, attached to a fine string, is swallowed. After swallowing, the capsule coating dissolves in the stomach to release a small brush which when removed allows cell collection from the lining of the oesophagus (gullet or food-pipe). These cells are then analysed for abnormalities. The procedure is used to identify important oesophageal conditions such as Barrett’s oesophagus.
Identifying cell changes in screening is important to ensure conditions such as Barrett’s do not progress to become oesophageal cancer.
Q. Where is Capsule Sponge available?
A. Capsule sponge is currently only available in Leigh Infirmary, Salford Royal Hospital and Royal Oldham Hospital. As we are still in the pilot stage, it is not available across the whole of Greater Manchester.
Q. Who is eligible?
A. People with symptoms of reflux who have been referred by their GP on a diagnostic upper GI endoscopy pathway. A gastroenterologist or endoscopy nurse will triage patients for capsule sponge and will contact eligible patients directly.
Q. I’m a healthcare professional who would like more information about the programme, who should I contact?
A. Thank you for your interest in the pilot. If you would like any additional resources or information, please contact s.walker21@nhs.net
Lynch Syndrome is a genetic condition that increases risk of certain cancer types, including colorectal cancer and endometrial cancer. NICE guidance states that all colorectal cancer and endometrial cancer patients should be tested for Lynch Syndrome. This test is performed on a sample of the tumour collected in a biopsy.
Greater Manchester Cancer Alliance is working in collaboration with the North West Genomics Medicine Service Alliance to increase the amount of Lynch Syndrome testing for all colorectal and endometrial cancer patients across Greater Manchester.
Lynch champions were appointed in each colorectal and endometrial MDT. The role of a Lynch champion is to ensure universal testing for Lynch Syndrome for newly diagnosed patients. They also ensure that patients are offered or referred for downstream genetic testing, where appropriate.
For further information on Lynch Syndrome testing, please visit:
Q. Where is Lynch Syndrome testing available?
A. All NHS Trusts in Greater Manchester should test for Lynch Syndrome following a diagnosis of colorectal cancer or endometrial cancer.
Q. I’m a healthcare professional who would like more information about the project, who should I contact?
A. Thank you for your interest in this project. If you would like any additional resources or information, please contact s.walker21@nhs.net
Programme Governance
Early Diagnosis Programme Board
The Early Diagnosis Programme Board oversees the delivery of the Early Diagnosis Programme
See the range of organisations represented:

Senior Team

Dr Sarah Taylor
Associate Medical Director for Early Diagnosis and Primary Care

Ali Jones
Director of Cancer Commissioning and Early Diagnosis
Project Managers
Mike Armstrong
Lung Pathway Improvement Manager

Oliver Butterworth
Targeted Lung Health Check Project Manager

Sophie Walker
Pathway Improvement Manager
Primary Care Team

Paul Keeling
Primary Care Project Manager
Andrew Beaney
Primary Care Facilitator
Hannah Dixon
Primary Care Facilitator
Hannah Morris
Primary Care Facilitator
Sue Sykes
Primary Care Facilitator
Health Inequalities

Dan Clark
Health Inequalities Project Manager