Personalised Care
Personalised care is fundamental to delivering better quality care that is meaningful to the individual and supports their health and wellbeing. This empowers people to manage their care and the impact of their cancer.
Everyone is different and will have different concerns when they are diagnosed with cancer. We are working to make sure that people with cancer are treated as people. Every patient should have the opportunity to discuss all of their concerns, whether during a hospital appointment or with their GP, and get the support they need.
Personalised Care Programme Board
The Personalised Care Programme Board was established in 2023.
The Board brings together the key stakeholders from across Greater Manchester who are responsible for the delivery of personalised Care in Cancer services. This includes representation from primary and secondary care services as well as commissioners, public health and patient and carer representatives from our Cancer Voices Community. The Board also includes representation from 10GM which supports this programme to engage with Voluntary, Community and Social Enterprise (VCSE) organisations across Greater Manchester.
The Programme Board will report to and be held to account by the Greater Manchester Cancer Board.
Key people

Michelle Leach, Live Well with Cancer Programme Manager

Katie Law, Programme Manager for Genomics/Psychological Support

Andrea Webber, Core Interventions Project Manager

Simran Chandler, Genomics Project Manager

Lisa Heys, Genomics Project Manager

Olivia Gunby, Personalised Care Manager, Psychological Support & Mental Health

Max Thomasson, Personalised Care Project Officer
What do we mean when we say “Personalised Care”?
Personalised care simply means that patients have more control and choice when it comes to the way their care is planned and delivered, taking into account individual needs, preferences and circumstances.
Due to developments in diagnosis and treatment of the disease cancer survival rates have doubled in the last 40 years. There are currently 2.5 million people living with cancer in the UK however this is set to rise to 4 million by 2030. This means more people are living with the disease, its side effects and the consequences of its treatment for many years.
Listen to Farida’s story and what Personalised Care means to her
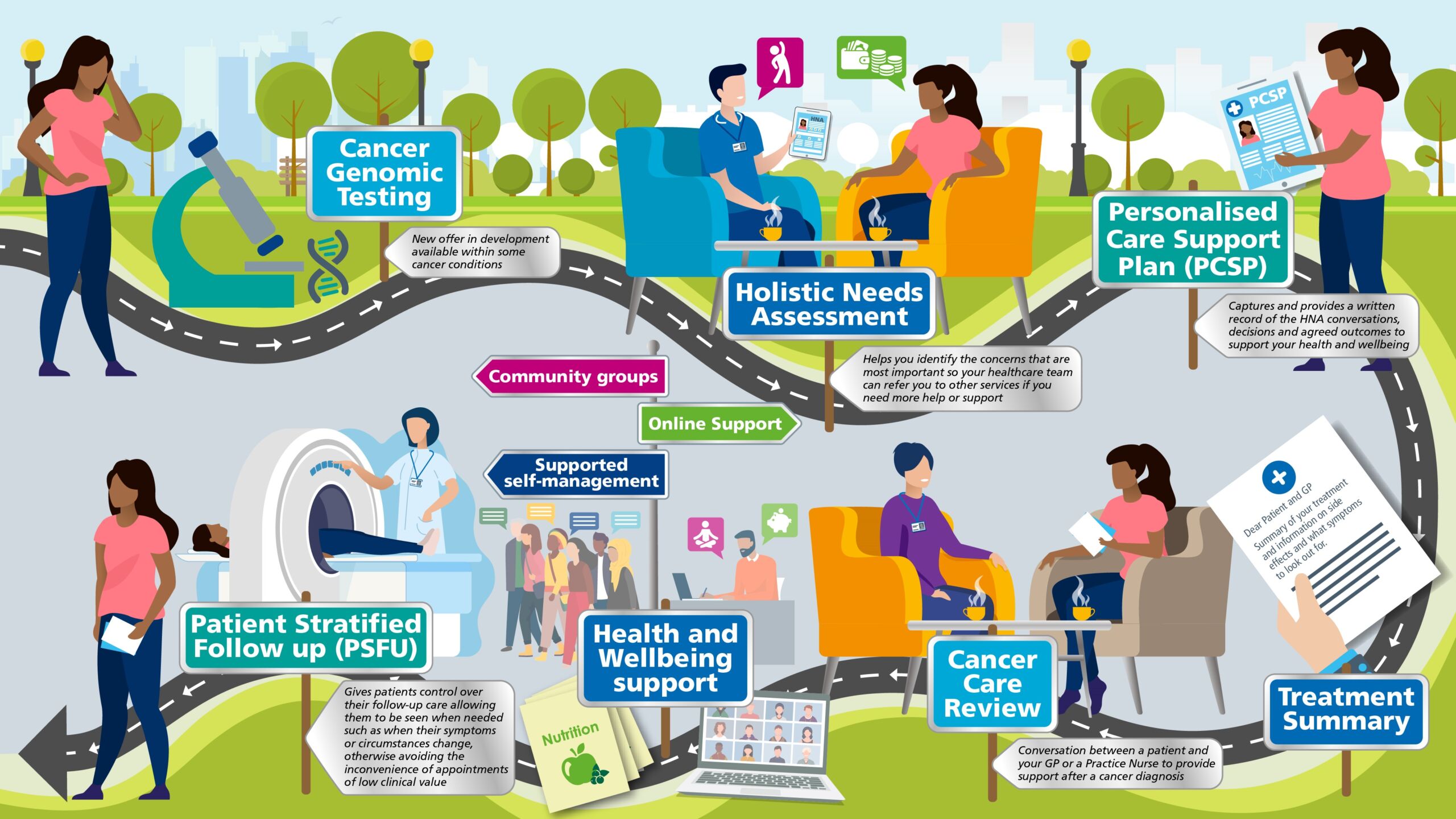
The map below shows what patients should be offered throughout their pathway to ensure they receive personalised care.
Our Personalised Care Programme will be supporting and driving forward the quality delivery of this pathway that should be available for all patients diagnosed with cancer.